Tricia Cresswell on women’s reproductive rights, then and now
Tricia Cresswell, author of The Midwife, reveals the uneven progress of women's reproductive rights across the world and highlights the ongoing risks to the rights of pregnant women.
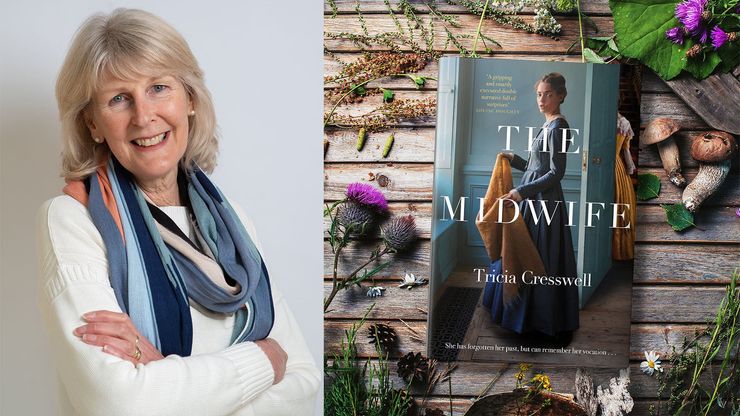
Tricia Cresswell's Victorian drama The Midwife plunges the reader into a rich imaginative world, with the parallel stories of a woman found after a storm – who can remember little but how to heal a wound and deliver a child – and a respectable doctor with a deep secret. Haunting and moving in equal parts, the book details the medical difficulties of giving birth in the 1800s, and contains a strong message about women's place in society and the role of female practitioners.
Here Tricia, a retired doctor and more recently a volunteer vaccinator, gives us the stark facts about women's reproductive rights across the world, both in the mid-nineteenth century when her novel is set, and our present day.
The Midwife is set in England around 1840. It is a work of fiction, but I wanted to capture something of the essence of the period. It was a time of massive social divide between the rich and the poor, and rapid change as the new industries displaced many traditional ways of life. Marriage was the social norm across all classes. It was assumed that wives would become pregnant, and being ‘barren’ was seen as an exclusively female problem. Pregnancy was both a required duty and a source of real fear.
In 1840, the UK maternal death rate is estimated to have been around 700/100,000 live births, meaning that one woman died for every 143 babies born. Due to the high pregnancy rate (women gave birth to an average of eight live or stillbirths in their life), the estimated lifetime risk of death in childbirth was 1 in 20!
‘We have reproductive rights. But, many women across the world are still without this necessary support and vital services. They do not have these reproductive rights. ’
The stark reality was that every family would know a woman who died in pregnancy or childbirth. These women died of obstructed labour, infection, blood loss or following unsafe abortion.
Since then, there have been massive improvements in pregnancy outcomes. In 2017, the UK maternal death rate was 8/100,000 live births. Maternal death is now a rare tragedy, and the vast majority of us who become pregnant do so with very little fear for our own lives and the realistic hope of a healthy baby. This is thanks to many interacting factors. We are well-nourished and healthier, we have choice, we have access to free midwifery and obstetric care. We have antisepsis and antibiotics, blood transfusion and caesarean section, contraception and safe abortion.
We have reproductive rights.
But, many women across the world are still without both this necessary support and vital services. They do not have these reproductive rights.
In 2017, by WHO (World Health Organisation) region, the lowest maternal mortality rate was Europe (13/100,000) and the highest was seen in Africa (526/100,000). Meaning that maternal death rates in parts of Africa today are not much better than in the UK in 1840.
‘Maternal death rates in parts of Africa today are not much better than in the UK in 1840. ’
As Dr Geeta Rao Gupta, deputy executive director of UNICEF, said in 2014, ‘a 15-year-old girl living in sub-Saharan Africa faces about a 1 in 40 risk of dying during pregnancy and childbirth during her lifetime. A girl of the same age living in Europe has a lifetime risk of 1 in 3300 – underscoring how uneven progress has been around the world.’
The concept of women’s reproductive rights did not become fully articulated as an essential component of female emancipation and equality until the 1970s. Fifty years on, issues related to women’s reproductive rights are some of the most deeply contested rights worldwide.
In some societies, marriage and repeated pregnancies remain the social norm, with no access to effective contraception or safe abortion, due to religious or cultural prohibitions. In a small number of societies, female genital mutilation is still practised which can lead to obstructed labour and other problems such as fistulae, recurrent bladder infection and kidney damage. And worst of all, in recent terrible conflicts, women are still being systematically raped as an act of war.
What’s more, access to safe abortion remains a contentious issue. It was only last year that women in Northern Ireland, after a long and bitter struggle, secured access to services, 50 years after the rest of the UK. There were also major successes in the legalising of abortion in Argentina, South Korea, Mexico, Nepal, Benin and San Marino.
Tragically, this real progress is being overshadowed across the world by increasing attacks on women’s reproductive rights. Poland banned abortion in January 2021 and Slovakia restricted access to abortion services. In the USA, the recent Texas State Senate Bill 8 effectively banned most abortions from six weeks of pregnancy in the state. The US Supreme Court then ruled to keep that law in place. Other states are introducing similar restrictive laws. There is now a real possibility that the landmark Roe v. Wade judgement, which underpins abortion rights in the USA, may be overturned.
Former President Trump’s expanded ‘Global Gag Rule’ in 2017 blocked US global funding to organisations providing information, referrals or services for legal abortion in their own countries. Although this policy was rescinded by President Biden in January 2021, its impact in poorer countries was enormous and has led to the collapse of many local contraceptive and maternity services for women.
‘We know that once girls and women have access to education and contraception, numbers of pregnancies fall and overall community health improves, even in the poorest countries. It is that simple.’
What really matters is this. We know how to reduce maternal and infant deaths. The three essential components are:
- The general education of girls and women
- The local provision of services for girls and women: contraception; safe abortion; care during pregnancy, during labour and after childbirth
- The local provision of infant and child health services
We know that once girls and women have access to education and contraception, numbers of pregnancies fall and overall community health improves, even in the poorest countries.
It is that simple.
Yet, in 2021, the UK overseas aid budget was reduced, defunding projects supporting the development of these services in some of the poorest communities in the world. And in Afghanistan, we watch now as girls’ and women’s so very hard-won rights are being stolen away. We need to protect our reproductive rights here in the UK and we need to support girls and women across the world. We can start by lobbying our MPs about the overseas aid budget. We can start by supporting campaigns and charities which explicitly promote women’s rights to contraception, safe abortion and maternity care. Underpinning all of this is the education of girls. Knowledge is power.
For more information see:
https://www.who.int/news-room/fact-sheets/detail/abortion
https://www.who.int/news-room/fact-sheets/detail/maternal-mortality
https://www.ippf.org/blogs/2021-sexual-and-reproductive-health-and-rights
The Midwife
by Tricia Cresswell
1838. A violent storm has hit the Northumberland coast, and a woman is found alone, naked and on the verge of death. She has no memory of how she got there, but she can speak fluent French, dress a wound and help women give birth. She starts to rebuild her life, helping those around her and finding a fragile happiness. Until tragedy strikes and she must go into hiding. Meanwhile in London, respectable Dr Borthwick assists mothers and babies in high society, and in the slums of Devil's Acre. The solitary doctor has a secret though, one which threatens to engulf him . . .