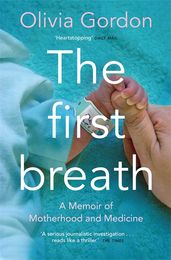
Synopsis
‘Fascinating and moving.' - Adam Kay, author of This is Going to Hurt
A BBC Radio 4 A Good Read choice
This is a story about the cutting-edge medicine that has saved a generation of babies.
It's about the love and fear a parent feels for a child they haven’t yet met.
It's about doctors, mothers, fathers and babies as together they fight for the first breath.
The First Breath is a book about motherhood and medicine.
Olivia Gordon decided to find out how, exactly, modern science saved her son’s life. Crossing medical memoir with popular science, The First Breath is an investigation into the pioneering fetal and neonatal care bringing a new generation into the world, who would not have lived if they had been born only a few decades ago.
The First Breath explores the female experience of medicine and details the relationship mothers develop with doctors who hold not only life and death in their hands, but also the very possibility of birth.
From the dawn of fetal medicine to neonatal surgery and the exploding field of perinatal genetics, The First Breath tells of fear, bravery and love. Olivia Gordon takes the reader behind the closed doors of the fetal and neonatal intensive care units, resuscitation rooms and operating theatres at some of the world’s leading children’s hospitals, unveiling the untold story of how doctors save the sickest babies.
Details
Reviews
Fascinating and moving.
Excellent . . . A serious journalistic investigation into foetal and neonatal medicine . . . reads like a thriller.
Heartstopping
A triumph of memoir-cum-non-fiction and a love story starring our heroes, the NHS . . . Totally brilliant and touching . . . tender, well researched and unputdownable, the best book I've read in the last twelve months. [The First Breath] moves effortlessly between personal stories of children and cutting edge scientific research . . . [Gordon makes] us feel the great and risky adventure of surviving a difficult childhood and becoming a person: and the linked one of being a parent . . . a wonderful, intelligent writer.